Request a video call
Confirm Your Virtual Consultation
Lakshmi Neuro Clinic | Dr. Ramnarayan | Neurosurgeon Profile Overview
Dr Ramnarayan has wide experience in general neurosurgery like brain tumours, disc surgery etc. He is also trained in functional neurosurgery, a new subspecialty which is concerned with the treatment of conditions like chronic pain (including cancer pain and failed back surgery syndrome), spasticity, movement disorders (Parkinson's disease, dystonia, tremor etc), psychiatric conditions and epilepsy and recently addiction is being added as an indication.
Dr Ramnarayan has also visited many international neurosurgical centres like the University of Pittsburgh, University of California, San Francisco, University of Geneva, Malaya University etc. Dr Ramnarayan also has a good number of international publications some of which are widely quoted and many national and international presentations.
We offer treatments for the following:
General neurosurgery:
- Surgery for tumours of the brain and spinal cord,
- Disorders of the blood vessels of the brain like aneurysms,
- Surgery for strokes including putaminal haematoma
- Spinal problems like disc prolapsed.
- Neurological problems in children like brain tumours, congenital defects like meningocoel and hydrocephalus
Functional neurosurgery:
- Intrathecal drug delivery systems for pain including cancer pain, failed back syndromes and spasticity due to various causes.
- Spinal cord stimulation for
1. Failed back surgery syndromes (FBSS)
2. Refractory angina pectoris (RAP)
3. Intractable Diabetic neuropathy.
4. Peripheral vascular disease pain (PVD)
5. Complex regional pain syndromes (CRPS I & II)
6. Brachial plexus injury pain.
7. Trigeminal neuropathy.
8. Post amputation/phantom limb pains
9. Post herpetic neuralgia. - Surgery (DBS) for movement disorders like Parkinsonism and dystonias.
- Surgery for epilepsy including vagal nerve stimulation.
- Surgery (DBS) for psychiatric disorders like Intractable obsessive compulsive neurosis, Intractable depression and Tourettes’ syndrome.
- Surgery for addiction like alcoholism.
Dr Ramnarayan is a member of various professional organisations including:
- Life Member of the Neurological Society of India (NSI)
- International member of the American Association of Neurological Surgeons (AANS).
- Member of the Indian Medical Association, Kerala Chapter, India.
- Life Member in Neurological Society of India (Kerala Chapter).
- Member of the Indian Medical Association, Tamilnadu Chapter, India.
Please Click here to request more information from Dr Ramnarayan.
Lakshmi Neuro Clinic | Dr. Ramnarayan | Neurosurgeon Treatments Offered
What is Functional Neurosurgery?
Functional neurosurgery is concerned with the treatment of conditions where the central nervous system (brain and spinal cord) physiology (normal function) is altered but the anatomy may or may not be normal. Examples of conditions treated by functional neurosurgery are chronic pain (including cancer pain and failed back surgery syndrome), spasticity, movement disorders (Parkinson's disease, dystonia, tremor etc), psychiatric conditions and epilepsy etc. Recently addiction is being added as an indication.
Pain is probably the commonest symptom for a multitude of diseases starting from tension headache to malignant tumours. Pain is of two types: acute and chronic. Acute pain is of limited duration and is well controlled by pharmacological measures. Chronic pain is of longer duration and persists long after the initial injury. When pain persists or recurs for more than six months, it is definedas chronic pain. It requires pharmacological, psychological and even surgical measures to control the pain. Such pain no longer serves a useful purpose and can cause severe psycho-socio-financial effects. Normal living becomes severely restricted or even impossible and can lead to much suffering on the part of patient and family. Patients go from doctor to doctor or worse self medicate but never get cured. Most of these medicines can affect the heart and kidneys if used repeatedly. Unfortunately in our country pain is not being given the importance it deserves.
Treatment of pain is always conservative and pharmacological initially; later physical and occupational methods are tried; only if all these conservative methods fail should surgery be planned. The dictum would be to always look for the cause of the pain and if any cause is found, treat this cause. If conservative methods fail/does not produce desired effect, then more invasive procedures include corrective surgery (eg discectomy), anaesthetic techniques (IC block), Neurostimulation/ intrathecal drug delivery system and as a last resort neuroablative procedures may be needed. Treatment is done in a series of steps starting from simple drugs to oral opiods. Adjuvant drugs like antidepressents are added as and when indicated. Other measures like physiotherapy, nerve blocks etc form part of the armamentarium. Most patients need only these but in 15 – 20% of patients these measures are not effective or they have a high incidence of side effects. Advanced therapies are indicated in these cases.
These include:
- intrathecal drug delivery
- neurostimulation,
- neuroablative therapies
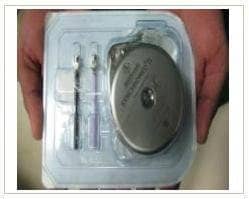
Intrathecal drug delivery systems
Intrathecal drug delivery systems can deliver drugs like morphine or baclofen directly into the intrathecal space which contains CSF so that the drugs act directly on receptors in spinal cord. The main advantages are that the dose of drug required is about 1/200th of oral dose, so side effects like constipation/drowsiness does not occur. There is no systemic absorption so no problem with tolerance and addiction liability. Many studies have shown that this procedure is effective in reducing pain in more than 80% of patients with a very good safety profile.
Intrathecal morphine indicated:
- diffuse cancer pain
- failed back surgery syndrome,
- osteoporotic pain,
- neuropathies like brachial plexus injuries and other painful neuropathies etc.
Intrathecal baclofen is indicated in spasticity due to cerebral palsy, spinal cord injury, multiple sclerosis, brain hypoxic injury, severe head injury, and metabolic diseases. Many studies have shown that Intrathecal baclofen has significant and worthwhile functional benefits and acceptable cost / benefit ratio. The results are very good especially in cerebral palsy children with a good intelligence quotient, multiple sclerosis and spinal cord injury with severe flexor spasms. Another innovation is using intrathecal baclofen for patients in persistent vegetative state and isolated case reports have shown that most patients benfit and achive a good level of consciousness. Recently the pump has been used to deliver intrathecal thyroid regulating hormone (TRH) for chronic depression.
Spinal cord stimulators
Spinal Cord Stimulator is indicated in failed back surgery syndrome, peripheral neuropathies like intractable diabetic neuropathy pain and brachial plexus injuries, intractable angina pectoris, complex regional pain syndromes, pain due to peripheral vascular disease, radiculopathies like pain in the arm, phantom limb pain (after amputation), neuralgias like trigeminal neuropathies etc. The method involves introducing stimulating electrodes in the dorsal extradural space of the spinal cord. Many studies have shown that this is very effective in 60 – 80% of patients. The results have been very good in failed back syndromes, intractable angina especially after coronary artery bypass grafting, intractable diabetic neuropathy, and brachial plexus pain.
The most common indications for spinal cord stimulation includes:
- Failed back surgery syndromes (FBSS)
- Refractory angina pectoris (RAP)
- Diabetic neuropathy
- Peripheral vascular disease (PVD)
- Complex regional pain syndromes (CRPS I & II)
- Brachial plexus injury
- Trigeminal neuropathy
- Post amputation/phantom limb pains
- Post herpetic neuralgia.
Failed back surgery syndrome (FBSS)
SCS is used maximally for FBSS which is persistent or recurrent pain, mainly involving the lower back and/or legs, even after previous anatomically successful spinal surgery. A number of controlled studies and case series, some with as much as 10 years of follow up, have been performed to assess the efficacy of SCS in reducing the pain associated with FBSS. In one randomized controlled study, researchers compared SCS to repeated operation in patients with FBSS and found that significantly more patients receiving SCS (47%) achieved 50% or more pain relief compared with those who underwent repeated operation (12%; p , 0.01). A meta-analysis of the 72 case studies of patients in whom SCS was used to treat refractory neuropathic back and leg pain or FBSS showed that 62% of patients with SCS achieved 50% or more pain relief.
Refractory Angina Pectoris
Refractory angina pectoris is defined as “a chronic condition characterized by the presence of angina, caused by coronary insufficiency in the presence of coronary artery disease, which cannot be adequately controlled by a combination of medical therapy, angioplasty, and coronary artery surgery. Spinal cord stimulation is one of the most promising treatment options for this disease. Prospective randomized controlled studies of SCS showed benefits both in QOL and cardiac indices, exercise duration and time to angina significantly increased in the SCS group compared with the controls and nitrate consumption, ischemic episodes at rest and with exercise, and pain significantly decreased. In the ESBY study, 104 refractory angina patients randomized to SCS (53) or CABG (51). Results (at 6 months’ follow-up) showed cardiac mortality significantly lower in SCS group (1) compared to CABG group (7), neurostimulation and CABG were equivalent methods in terms of symptom relief and CABG was superior during exercise testing but cerebrovascular events less with SCS. The conclusion was that SCS may be a therapeutic alternative for patients with increased risk of surgical complications.
Peripheral Vascular Disease
Peripheral vascular disease can lead to critical limb ischemia. Spinal cord stimulation is indicated when critical limb ischemia becomes inoperable and has shown a significant effect in alleviating pain, but several controlled trials have shown limited benefits on limb survival. A Cochrane systematic review of the limb salvage data showed a significant treatment effect in favor of SCS after 12 months. There have also been some retrospective case series of patients with critical limb ischemia associated with Buerger disease and end-stage renal disease, in which investigators have suggested that SCS may also be useful in these patient subsets.
Complex Regional Pain Syndrome
The CRPS’s can be divided into Types I and II. In CRPS Type I, formerly called reflex sympathetic dystrophy, no known nerve injury is present. In CRPS Type II, formerly called causalgia, a known nerve injury is present. The use of SCS has been shown to be effective in helping restore normal function in affected limbs, especially if used early in the course of the disease. Specifically, if patients do not respond to conventional treatment within 12 to 16 weeks, a trial of SCS should be considered.Generally, SCS has been shown to be highly effective in the treatment of CRPS with 67% of patients with CRPS Type I or II who underwent implantation of an SCS device achieved pain relief of 50% or more and that the QOL was significantly improved.
Diabetic peripheral neuropathy.
Many studies have shown the positive effect of SCS in intractable diabetic neuropathy. In a study of 30 patients with SCS for neuropathy, at 87 months' follow-up, 14 achieved long-term success in control of chronic pain. 6 reported excellent relief (> 75%), 8 had good relief (> 50%), and six had poor relief (< 50%). In another study, 10 diabetic patients who did not respond to conventional treatment, 8 had statistically significant pain relief with the electrical stimulator. A recent study in which 11 diabetic patients with chronic pain in their lower limbs and no response to conventional treatment were studied. At the end of the study, 8/9 patients continued to experience significant pain relief and for six of them, the stimulator was the sole treatment for their neuropathic pain.
SCS in brachial plexus injury
The pain due to brachial plexus injury is one of the most miserable even leading to suicide. Many studies have shown the effectiveness of SCS. One study compared SCS with DREZotomy and concluded that SCS is more effective in patients with partial root avulsion or intact roots, nevertheless the success rate is unpredictable. Therefore SCS remains the first choice of treatment, especially due to its relative non-invasive technique when compared with DREZ lesions.
Deep brain stimulation (DBS) for chronic pain
This is another recent advance for treatment of chronic pain. Different forms of neuropathic and mixed nociceptive/neuropathic pain syndromes can be treated with DBS. Electrodes are implanted in the somatosensory thalamus and the periventricular gray region. The best long-term results are attained in patients with FBSS and CRPS.
Motor cortex stimulation for chronic pain.
Motor cortex stimulation (MCS) is a treatment option for central deafferentation pain and for trigeminal neuropathic pain when less invasive interventions fail. Only the most refractory patients suffering from the most disabling pain syndromes are deemed candidates for MCS. Encouraging results with MCS have been reported. successful outcomes in the majority of the 12 patients with central pain secondary to intracerebral hemorrhages and infarcts but those with trigeminal neuropathic pain (TNP) or peripheral neuropathies had better outcomes.
Surgery for movement disorders
Movement disorders are neurological conditions that affect the speed, fluency, quality and ease of movement. Abnormal fluency or speed of movement (dyskinesia) may involve excessive or involuntary movement (hyperkinesia) or slowed or absent voluntary movement (hypokinesia). Common examples include Parkinsonism, various types of dystonis like spasmodic torticollis. The commonest movement disorder is Parkinson’s disease which manifests with tremors, rigidity, slow movement (bradykinesia), poor balance, and difficulty in walking. It affects 1 – 2% of people above 60 yrs but in India it is seen in younger people also (upto 15%). A recent study has reported that India is among the countries where the incidence of Parkinson's disease is expected to double by 2030. Treatment of movement disorders like Parkinsonism is predominantly by drugs and is very effective in most cases. But a good number of patients either come out of good control in the long term or develop side effects of the drugs used. Such patients are surgical candidates and presently the surgery for Parkinsonism with the widest acceptance is subthalamic nucleus (STN) deep brain stimulation (DBS). The difference between stimulation and ablation are that brain stimulation effects are modifiable and are reversible. But ablation is permanent and not modifiable. So ablative surgeries are not much practiced nowadays.
Indications for DBS in Parkinsonism
- Advanced Parkinson’s disease with disabling motor fluctuations and dyskinesias refractory
to drug changes. - Levodopa induced dyskinesias.
- Medication refractory symptoms with significant disability and interference with daily
activities including writing, feeding, dressing, etc. - No significant cognitive impairment and no major psychological problems.
10 years after diagnosis. - Patients understand and accept therapy.
- Parkinson”s Disease can be said to be having three stages.
- Stage 1 is early PD where most of the people can be managed with medical treatment ; however 20% of the patients (especially with tremors) who do not respond to conservative treatment can be offered surgery.
Stage 2 of PD is where medical treatment starts loosing its efficacy, is associated with side effects like hallucinations and dyskinesias and causes wide fluctuations of on and off and dyskinetic state. Surgery is very useful at this stage. This stage occurs after 5 or more years of disease. Besides dyskinesias and motor fluctuations, other indications include severe pain and hallucinations. Stage 3 of PD is the most advanced stage when the patient is virtually bed bound and barely responds to medical treatment, and has significant side effects. Surgery may or may not be possible in this case.
Deep brain stimulation (DBS) for Parkinsonism involves stimulating the subthalamic nucleus (STN) (figure 4) with the electrodes shown above (figure 3A &B). For dystonias the target is the globus pallidus (Gpi). Surgery for Parkinsonism usually resolves tremor, dyskinesias, pain and hallucinations. Symptoms which are improved by drug therapy are maximally improved with surgery. Tremor improves by 80%-100%, slowness (Bradykinesia) by 50%-60%, stiffness (Rigidity) by 50%-70%, gait, freezing, and balance by 50%, dyskinesias and dystonia (drug induced) by 80%- 90% and motor fluctuations are virtually eliminated. Independence and quality of life are substantially improved. Complications include haemorrhage (2-3%), Infection (1 -3%), mechanical hardware breakage (1-5%) and cognitive decline (2%) but are very rare.
Dystonias are of many types: unifocal or multifocal, segmental and generalized based on presentation and may be idiopathic or secondary based on aetiology. The initial management is always medical. Botulinium toxin is effective in localised dystonia like cervical dystonia.
Dystonias become resistant to medical management and so surgical options need to be explored. Many procedures are done like sectioning of spinal accessory or sternocleidomastoid in cervical dystonia. Bilateral Globus pallidus interna (Gpi) deep brain stimulation (DBS) is very effective for most intractable dystonia. Visual evoked potentials are done during Gpi DBS.
Surgery for epilepsy
Epilepsy is a condition characterized by the occurrence of seizures and transient alterations in consciousness resulting from abnormal electrical activity in the brain. The main treatment of epilepsy is always medical but in patients who are unresponsive to or are intolerant to medical therapy, surgery becomes an option. It is very important to determine that all medical options have been exhausted prior to surgery. Usual surgical procedures include resective (removing portions) surgery like lesionectomy, temporal lobectomy, corpus callosotomy, hemispherectomy. Another recent advance is vagal nerve stimulation.
Temporal lobectomy is the most common surgery for epilepsy. Complex partial seizures of temporal lobe origin constitute 25% of all epilepsy and among this a third is refractory to medical management. Indications for temporal lobectomy include intractability to medical management and concordance of clinical, radiology, electrophysiological and neuropsychological data. Structures removed (based on above) include anterior lateral temporal neocortex (4cm), anterior 3 cm of parahippocampal gyrus, hippocampus and amygdala. The results are usually good with upto 70% becoming seizure free and upto 20% getting improvement in seizure controll.
Hemispherectomy is indicated in partial seizures with contralateral hemiplegia interfering with neurodevelopmental milestones and a resectable epilepticogenic focus. Eg. Sturge Weber syndrome, Ramussens encephalitis, infantile hemiplegic epilepsy etc. Structures removed include the frontal, parietal, occipital and lateral temporal lobes. With complete hemispherectomy, upto 85% of patients achieve a seizure free status. Postoperatively CSF pathway obstruction can occur necessitating a shunt.
Multiple subpial resection is indicated when the seizure focus is at or extending into eloquent cortex. The principle of this procedure is that vertical transection of eloquent cortex does not produce any deficits. The main Indications include:
- focus in eloquent cortex
- Landau-Kleffner syndrome (epileptic aphasia)
- Epilepsia partialis continua
- Failed hemisperectomy in Rasmussens.
Multiple resections are done using the subpial transection hook. The results are usually good and 75% of patients with intractable seizures have upto 90% improvement.
Corpus callosotomy involves division of corpus callosum to prevent spread of seizure discharge. This will help in preventing secondary generalization of the seizures. The main indications include poorly controlled generalised seizures but no primary focus can be demonstrated eg: Lennox- Gastaut syndrome, multi centric CPS with secondary generalization. Complete sectioning of corpus callosum is essential for good results; 80% 0f patients reported more than 50% reduction in seizure frequency. Sequele include reduced spontaneity of speech, non dominant limb apraxia which are transient and interhemispheric sensory dissociation.
Vagal nerve stimulation is a new method being used because not all patients with medically refractory epilepsy are candidates for resective surgery. Resective surgery is not always an option for medically refractory seizures. Vagus nerve stimulation (VNS) is an adjunctive treatment for certain types of intractable epilepsy and major depression. Vagus nerve stimulation (VNS) is designed to prevent seizures by sending regular, mild pulses of electrical energy to the brain via the vagus nerve. Indications include patients who have failed surgery before, patients who require extratemporal surgery in eloquent area or corpus callosotomy or the patients’ choice.
Psychoneurosurgery
Neurosurgery was used for psychiatric procedures in the 1970’s but with the advent of good neurpharmacology this slowly went into disfavour. However with the introduction of new techniques and equipments, both stimulation (DBS) and ablation procedures are being used again. As mentioned earlier, ablative procedures are slowly losing favour because of reasons mentioned earlier.
The main indications for DBS in psychosurgery include:
- Intractable obsessive compulsive neurosis
- Intractable depression
- Tourettes' syndrome.
- A recent addition is giving TRH intrathecally using intrathecal drug delivery systems which produces good results in refractory depression.
Deep brain stimulation for Addiction.
Another recent introduction is deep brain stimulation (DBS) for addiction. PET scan studies have shown that when an individual takes a psychoactive substance, dopamine is released in the nucleus accumbens, which causes "the high". By an increased dopamine release in the nucleus accumbens, the inhibition of the output neurons is decreased, which causes activation of the reward system. Case reports have shown that DBS of nucleus accumbens causes reduction in alcohol, nicotine and heroin intake. Studies in lab animals have also shown the same results.
Please Click here to request more information from Dr Ramnarayan.
Lakshmi Neuro Clinic | Dr. Ramnarayan | Neurosurgeon Certificates, Accreditations, Qualifications Treatments Offered
Profile of Dr. R. Ramnarayan, Consultant Neurosurgeon and Functional Neurosurgeon
Qualifications
M.B.B.S: Medical College, Trivandrum, University of Kerala, India
M.Ch (Neurosurg), National Institute of Mental Health and NeuroSciences (NIMHANS). Bangalore, India.
Clinical attachment from Singapore General hospital.
Functional Neurosurgery Fellowship from the Walton Centre for Neurology and Neurosurgery, Liverpool, United Kingdom.
Current Position
Consultant Neurosurgeon
- Apollo Specialty Hospitals, Chennai, India
- Chettinad Multispecialty Hospitals, Chennai, India.
- Chennai Meenakshi Multispecialty hospital, Chennai
- Lifeline hospital, Chennai.
- Was holding academic post (Associate Professor of Neurosurgery) in a few Medical colleges (Latest SRM Medical College Hospital, Chennai).
Specialisation
Dr R. Ramnarayan is an experienced general neurosurgeon and also subspecialised as a Functional neurosurgeon.
General neurosurgery: surgery for the diseases of the brain and spinal cord. This includes
- Surgery for tumours of the brain and spinal cord
- Surgery for disorders of the blood vessels of the brain like aneurysms,
- Surgery for all types of strokes including putaminal haematoma,
- Surgery for spinal problems like disc prolapse,
- Neurological problems in children like brain tumours, congenital defects like meningocoel and hydrocephalus
Functional neurosurgery is a new subspecialty which is concerned with the treatment of conditions where the function of the brain and spinal cord is affected but the anatomy (structure) may or may not be normal.
Functional Neurosurgery Includes
- Surgery for chronic pain
- Intractable cancer pain
- Failed back surgery syndrome.
- Severe osteoporortic pain.
- Refractory angina pectoris
- Intractable diabetic neuropathy
- Peripheral vascular disease (PVD) pain
- Complex regional pain syndromes (CRPS I & II).
- Brachial plexus injury pain.
- Trigeminal neuropathy
Spasticity due to many causes like cerebral palsy, spinal cord injury, multiple sclerosis, brain hypoxic injury, severe head injury, and metabolic diseases.
Deep Brain stimulation surgery for movement disorders
- Parkinson's disease,
- Dystonia especially cervical dystonia
- Essential tremor.
Deep Brain stimulation for a few psychiatric conditions
- Intractable obsessive compulsive neurosis.
- Intractable depression.
- Tourettes' syndrome.
Surgery for intractable epilepsy.
- Ablative surgery like temporal lobectomy.
- Vagal nerve stimulation for epilepsy.
Deep brain stimulation for addiction like alcoholism.
Dr Ramnarayan is a member of various professional organisations including
- Life Member of the Neurological Society of India (NSI)
- International member of the American Association of Neurological Surgeons (AANS).
- Member of the Indian Medical Association, Kerala Chapter, India.
- Life Member in Neurological Society of India (Kerala Chapter).
- Member of the Indian Medical Association, Tamilnadu Chapter, India.
Dr Ramnarayan has also visited many international neurosurgical centres like the University of Pittsburgh, University of California, San Francisco, University of Geneva, Malaya University etc. He also has a good number of international publications some of which are widely quoted and many national and international presentations.
Publications
Original Articles
- Ramnarayan.R, Dominic A, Alapatt J, Buxton N. Congenital Spinal Dermal Sinuses: Poor Awareness leads to Delayed Treatment. Childs Nerv Syst. 2006; 22: 1220-1224.
- Ramnarayan R, Mackenzie I. Brain-stem Auditory Evoked Responses during Microvascular Decompression for Trigeminal Neuralgia: Neurol India 2006; 54: 250-254.
- Ramnarayan.R, Hegde T. Chronic subdural hematomas -- causes of morbidity and mortality. Surg Neurol. 2007; 67: 367-73.
- Ramnarayan. R, Dodd S, Das K, Heidecke V, Rainov. N.G. Overall survival in patients with malignant glioma may be significantly longer with tumors located in deep grey matter. J
- Neurol Sci. 2007; 260: 49-56.
- Ramnarayan R, Arulmurugan B, Paul Wilson, Rani Nayar. Twist drill craniostomy with closed drainage for chronic subdural haematoma in the elderly: an effective method. Clin Neurol
- Neurosurg. 2008; 110: 774 - 778.
- Ramnarayan R, Dominic Anto, Anilkumar TV, Rani Nayar. Decompressive Hemicraniectomy in large putaminal haematoma: An Indian Experience. J Stroke Cerebrovasc Dis. 2009:18: 1-10.
- Ramnarayan R, Praharaj SS, Jayakumar PN. Chiari-1 Malformations: An Indian Hospital Experience. Singapore Med J 2008; 49: 1029-1034.
Case Reports
- Ramnarayan. R, Sreehari N.R, Ninan G.K, John K M. Delayed Postoperative extradural haematoma: a case report. Pediatr Neurosurg 2007; 43: 113 -114.
- Ramnarayan R, Pazhanikumar C. Bilateral foot drop without cauda equinae syndrome due to L4-L5 disc prolapse: a case report. Internet Journal of Neurosurgery. 2008, Vol 5, No 1.
- Ramnarayan.R, Jeyanthi S. Postpartum cerebral angiopathy mimicking hypertensive putaminal haematoma: A case report. Hypertens Pregnancy. 2009; 28: 34 - 41.
Abstracts
- Ramnarayan.R, Dominic Anto, Alapatt .J, Buxton N: Congenital Dermal Sinus: Poor awareness leads to delayed treatment. Childs Nerv Syst. 2004, 20(4); 284.
- Ramnarayan.R, Mackenzie I, Forster A, Owen M, Eldridge PR, Varma TRK. The Effect of Changes in Auditory brainstem responses on hearing during Micro vascular Decompression for
- Trigeminal Neuralgia – An Assessment. Acta Neurochir 2004; 146(8): 890.
- Ramnarayan R, Dominic anto, Anilkumar T.V., Subbaiah M, Rani Nayar. Decompressive hemicraniectomy in large putaminal haematoma: an Indian experience. Can J Neurol Sciences 2007; 37 (Suppl): s51.
Please Click here to request more information from Dr Ramnarayan.

About Medical Center
- Speciality: Neurology, Robotic Surgery, Spine Care/Surgery
- Location: , Chennai, India
- Overview: Dr Ramnarayan has wide experience in handling all general types of general neurosurgery patients including patients with tumors of the brain and spinal cord, surgery for spinal problems like disc prolapse, congenital defects etc. He is also a functional neurosurgeon concerned with the treatment of conditions like chronic pain (including cancer pain and failed back surgery syndrome), spasticity, movement disorders (Parkinson's disease, dystonia, tremor etc), psychiatric conditions and epilepsy and recently addiction.









.png)






Share this listing